Hi there! The month of September is the sickle cell awareness month in the United Kingdom. I am particularly pleased to introduce to you a specialist in this area who has written an article exclusively for the Healthy Ebony Woman to create an awareness.
The following words are from Lara Odelusi who is an Advanced Specialist Nurse for Sickle Cell & Thalassaemia
Quality Improvement Strategic Lead
Table of Content
- Introduction
- Understanding Sickle Cell
- Prevalence
- Sickle Cell: A Deeper Look
- Impact On Women’s Health
Introduction
Sickle cell disease (SCD) is a genetic blood disorder that affects people worldwide and it can significantly impact lives of those diagnosed, including women. While both men and women can have SCD, women often face unique challenges due to the interplay of the disease with reproductive health and overall wellbeing. In this article, I delve into the specific effects of sickle cell on women’s health and explore ways to empower women with better care and support. The incidence of sickle cell is not gender related since it is an autosomal recessive disorder (hereditary). There is no difference in the rate of men and women with SCD as it is not a sex-linked disease.
Understanding Sickle Cell
Sickle cell disease (SCD) pose a global health challenge. It is the most common genetic disorder worldwide with 12,000 to 15,000 affected individuals in the United Kingdom (UK) alone.
SCD has its origins in sub-Saharan Africa and Middle East; hence, it is most prevalent in individuals of African descent as well as in Caribbean, Middle East, parts of India and Mediterranean, and south and Central America. Owing to population migration, SCD there are increasing numbers of affected individuals in Europe and the USA.
Prevalence / Incidence
-
- Sickle cell disease (SCD) affects 1:2000 live births (NHS sickle cell and thalassaemia screening programme 2020). See here
-
- Prevalence is increasing in the UK because of immigration into the country and new births.
-
- It is estimated that 300 babies are born with sickle cell disease in the UK every year and 300, 000 born per year globally.
-
- Seven percent of the world population are carriers of sickle cell disease.
Sickle cell: A Deeper Look
It is a serious genetic condition with two sickle cell genes inherited from both parents. It affects the red blood cells.
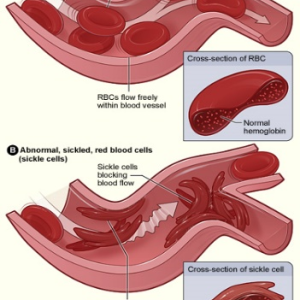
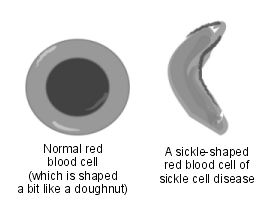
The red blood cells are naturally spherical (biconcave disks) in shape, contain special protein called the haemoglobin; this carries oxygen around the body. However, in individuals with SCD, their red cells are crescent- or “sickle”-shaped. Because of this, the red cells are less efficient in distributing oxygen around the body in people with sickle cell disease.
The crescent shaped red cells can become stuck in small blood vessels causing problems including pain; reduced oxygen supply to tissues around the body is contributory to the sickle cell pain.
The sickle red cells are destroyed more easily compared to the normal red blood cells. This means that people with SCD tend to have a lower number of red blood cells and lead to have a moderate and persistent anaemia.
People with sickle cell disease can suffer from anaemia and mild, moderate and or severe pain. These are known as crisis.
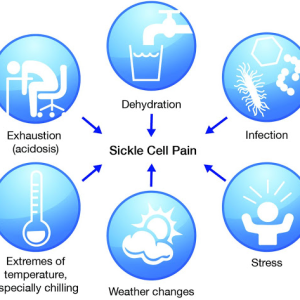
The painful crisis can be sudden onset of pain usually triggered by infection, stress, dehydration or weather changes.
Pain can be experienced in any part of the body: Joint pains, legs, arm, chest, abdomen, head.
Sickle cell trait is not the same as SCD or sickle cell disease. Sickle cell trait means you carry a single sickle cell gene, inherited from one parent but it does not normally cause illness.
The Impact on Women’s Health
Although sickle cell disease is not gender specific, women with SCD, encounter unique challenges. Let us have a look at some of them:
Menstrual irregularities: The chronic anaemia and low oxygen levels associated with sickle cell can disrupt hormonal imbalance, affecting the menstrual cycle; as a result, women with SCD could experience irregular menstrual cycles even amenorrhoea (absence of menstruation).
Pregnancy complications: Women with sickle disease require careful monitoring during pregnancy. The reduced oxygen getting to the baby could lead to growth restriction, premature birth, increased risk of maternal complications such as pre-eclampsia and infections.
Painful Crisis: SCD often causes pain episodes known as “crisis.” For women, this period of crisis can intensify during menstruation and pregnancy, adding an extra layer of discomfort and complications to their reproductive health.
Anaemia: SCD could cause the red blood cells to break down more rapidly than they can be replaced (haemolytic anaemia). Women may experience worsened anaemia during menstruation, leading to increased fatigue and weakness.
Iron overload: Some individuals with severe sickle cell disease sometimes require regular blood transfusions, which can lead to excess iron in the body. The excess iron could cause damage to organs such as the heart, liver, and endocrine glands.
Emotional and psychological impact: Living with a chronic illness can take its toll on the mental health. The effect can range from anxiety to depression or feelings of isolation and stress. Coping with chronic pain, managing fertility concerns and addressing pregnancy- related anxieties can be emotionally overwhelming.
Other challenges include:
-
- Delayed puberty growth,
-
- Bone and joint issues,
-
- Reproductive challenges- fertility and family planning.
-
- Difficult with employment and
-
- Stigma.
Joan, a 35-year-old lady, has lived with sickle cell disease since birth. Her story reflects the resilience and determination of a woman with sickle cell disease as she navigates the challenges posed by her condition.
She has experienced a fair share of frequent painful crisis, including regular hospital visits and admissions. Despite these challenges, Joan remains determined to lead a fulfilling life. She graduated from University with a First Class degree (although she had to defer her final year due to her sickle cell illness).
Joan went further with great resilience to pursue her career as a business analyst. She found an employer who is very supportive and offers her the opportunity to have a healthy work-life balance including being able to work from home, therefore accommodating her health needs.
Because Joan is determined to have a great quality of life with sickle cell disease, she follows her treatment plan strictly:
- Includes balanced and healthy diet
- Regular exercises
- Staying well hydrated.
- Getting prompt medical attention when required
- Taking all her prescribed prophylactic (crisis preventive) medication.
She has built a strong support network of family and friends who understands her limitations and provides emotional support when she requires it. Joan is an advocate and a member of voluntary group ‘Sickle cell warriors’. She engages in several seminars and talks promoting sickle cell awareness.
Pre Conceptual Care & Counselling
Pre-pregnancy counselling is crucial for women with SCD to discuss potential risks and plan for a safe pregnancy if desired.
Individuals are encouraged to find out their haemoglobinopathy status (genetic conditions affecting the haemoglobin part of the blood). This is especially needed if they are planning to start a family. Women and men with SCD or sickle cell trait are encouraged to have the statuses of their partners determined before they embark on pregnancy.
If the couples are ‘at risk’, for example, if both or either partners are carriers of sickle cell traits or affected by a major haemoglobinopathy, they should receive appropriate counselling regarding the risk of having affected offspring. The pre-pregnancy counselling and partner testing can be received via your General Practitioner (family Doctor) or genetic specialist.
It is particularly important to be aware of the methods of prenatal diagnosis and the potential risk of termination of pregnancy. In addition, it is imperative to be aware of the availability of preimplantation genetic diagnosis and request referral for this, if the couple desires it. Partners may not always be available or willing to undergo preconception testing. Women with SCD should be aware that if their partner’s status is unknown, the foetus should be treated as high risk for haemoglobinopathy. Sperm donors should also be screened for haemoglobinopathies for couples considering in vitro fertilisation (IVF).
Screening
Screening is usually done to find out if you are a carrier of sickle cell or thalassaemia gene and therefore likely to pass it on to your offspring. Those at high risk of being a sickle cell carrier are offered a test for sickle cell disease!
If the mother is found to be a carrier, screening is also offered to the father. The test should be offered before 10 weeks of pregnancy. If you find out you are a carrier, you and your partner will have the option of further testing to know if your baby is affected.
When both parents are carriers, each time they are expecting a child there’s:
- 1 in 4 chances of the child not having or carrying the disease.
- 2 in 4 chances of the child being a carrier.
- 1 in 4 chances of the child having the disease.
All newborn babies are offered testing for sickle cell and thalassaemia. Parents are informed of results, for babies who are identified as carriers of sickle cell or thalassaemia trait. Parents are given the results at birth.
The benefits of informing the parents of their baby’s result are so that they can inform their children when they are older for if and or when they plan to have children.
Sickle Cell and Pregnancy
During the antenatal screening, all women are offered sickle cell and thalassaemia screening as an integral part of antenatal care. There are approximately 100–200 pregnancies in women with SCD per year in the UK. It requires careful management and monitoring, and the management plan is tailored to the individual’s specific medical needs.
Here are some key points to consider:
- Pre-conceptual genetic counselling,
- Routine regular antenatal appointments
- Work closely with a health care team experienced in managing high-risk pregnancies and sickle cell disease.
- Provide effective pain management plan in managing sickle cell crisis, anaemia, and blood transfusion
Have you been affected by any of the things we have discussed here, or you are not sure of your genotype, your first point of call will be your doctor or Nurse Practitioner. If you have further questions you can send a direct email to the Healthy Ebony Woman.
Keep being amazing!
Yemisi x


