In my interaction with a few women recently, I have noticed a growing sense of weariness and hesitation around the use of hormonal contraceptives.
With a growing number of women now on hormonal contraception for various reasons, I would like to write this blog to give some balanced information so that women in this community can make informed choices.
The contraceptives get the job done pretty well without question if the right form is chosen for the right circumstances and used effectively.
TABLE OF CONTENTS
History of Contraception
Allow me to slide in a brief summary of contraceptive history before we head into the main discussion. Here is a snippet of some interesting information and to let us know that the use of contraception is an age-old phenomenon.
Around 2000 BCE, soaked soft materials like cotton or wool in mixtures of oils, fruit juice, herbs, and other substances created a tampon-like plug as a form of contraception.
Male and female condoms were known as sheaths in Ancient Egypt, Greek, and Rome. They were made from animal bladders and intestines, or from chemically treated linen.
During these times, the use of contraception was linked to illicit sexual relationships. They were only made available to married couples in the early 20th century.
It is fascinating to see how contraceptives have evolved over the decades. The first large-scale trial of the pill took place in 1956, and since then it has gone through more refined changes. Approximately 2.3 million women were using some form of oral birth control by 1963.
Combined contraceptives has two synthetic female hormones: oestrogen and progestogen ad can be in form of pills or patches.
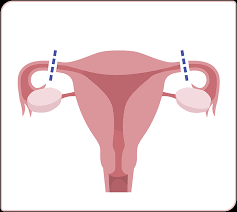
Progestogen contraceptives are available as pills, injectables, intrauterine system or subdermal implants.
Black Women And Contraception
Why is there a deeply rooted distrust of Black women in the women’s health aspect of the healthcare system?
In the 19th and 20th centuries, the Eugenics Movement pushed certain beliefs and practices in search for the perfect genetics to best represent the human race.
As a result of this, Black women in the United States were coerced into having fewer children by using sterilisation as a form of contraception. A lot of these women were sterilised without their consent.
The Latina and Puerto Rican women were also targeted for coercive sterilisation due to their ethnicity.
In my blog post on Female Genital Mutilation, young women slaves were cut and closed back up to prevent them from getting pregnant, thereby increasing their value in the slave market.
A few studies have shown that certain doctors persistently nudged black women into using contraception very early on.
And don’t forget, the risk of maternal deaths during pregnancy is four times higher in black women.
The ripple effect is increased disbelief in the healthcare system, especially in Women’s Health, hence low uptake of certain forms of contraception within these ethnic groups.
Health and Hormonal Benefits
Regardless of all the negative impact of the Eugenics movement, the use of contraception has its own advantages, including
- Lessened period pain
- Lighter period flow
- Improved premenstrual syndrome
- Reduced risks of ovarian and endometrial (lining of the womb) cancer with the use of combined contraception
- Less risk of uterine fibroid and endometriosis
- Improved acne
Contraceptive Side Effects

The pill made the news headlines recently when a new study was published: The use of progestogen-only hormonal contraception increases the risk of breast cancer as much as the combined contraception.
Yes, there is a small increased risk of Breast Cancer associated with the use of all hormonal contraception (not conclusive with the implants). This small risk is present as long as a woman is using them and goes away when they stop the contraception.
In practical sense, there are estimated 400 breast cancer cases attributed to pill use in the United Kingdom per year. On the other hand, approximately 4,400 breast cancer cases are caused by excessive and continuous consumption of alcohol.
Blood Clots risk in the deep vein is also slightly increased with the use of the oestrogen in the combined pills
Other notable side effects of hormonal contraceptives are usually mild and get better the longer you take them or switching to another form. The most common side effects of combined and progestogen-only oral contraceptive pills include:
Initial breakthrough bleeding, changes in menstruation and irregular bleeding are most common with the progestogen only pill or commonly called mini pills.
Progestogen only pills can cause acne flare up, on the other hand the combined pill helps to minimise or clear acne.
Nausea and Vomiting can be avoided by taking the pills at night before sleep.
Headaches and Migraines: If you are prone to hormonal headaches, this may get worse on the pill free week. This happens due to oestrogen withdrawal. Women on POP do not experience this. However, if you develop migraines while on the combined pill, then you should speak immediately with your healthcare professionals.
Hypertension: The combined oral contraceptive pills can increase blood pressure, which can lead to hypertension in 4-5% of healthy women. Hypertension can be exacerbated in about 9-16% of women with pre-existing raised blood pressure (BP). This is why it is important to check your BP regularly while on the pill.
Fertility usually returns within one to three months of stopping most hormonal contraceptives except for the progestogen-only injection, which may be delayed for up to a year.
In a study of women who used combined pills for one year, 97 percent of them had their periods within 90 days of stopping the pill.
Weight gain is not seen with the use of the new generation pills, however you can gain weight on the progestogen only injection. Simply due to increased appetite.
Vaginal Discharge could increase with the use of pills, this typically does not need treatment.
Sex Drive or libido could be reduced.
Mood changes: some ladies with PMS may find their symptoms improved with certain contraceptives
Coil Side Effects
- If adequate care is not taken by the professional inserting the coils, the uterus can be perforated. This is not a common occurrence.
- The uterus can perceive the coil as a foreign body and expel the device, most common in the first 6–8 weeks and during your period. Women who have never been pregnant are also prone to expel the coil. Don’t forget to always check for the strings after each monthly period.
- Cramps and bleeding are common in women who have the copper coil fitted.
- There is a higher risk of pelvic inflammatory disease (PID) in younger women with multiple sex partners. PID can also occur if the coil is inserted with untreated infection, such as chlamydia and gonorrhoea.
I suspect you may have questions after you have read this blog, please do not hesitate to reach out to me. Also, your healthcare professionals where individualised advice can be offered. So much appreciate you for stopping by my blog site once again!
Much love
Yemisi x



I just like the helpful information you provide in your articles